Ever thought how a minor liver issue could turn into something deadly? The journey from fibrosis to cirrhosis is important but slow. Liver fibrosis can get worse, turning into cirrhosis where permanent damage occurs. It’s vital to catch it early for a chance to reverse the effects. Knowing how liver scarring happens helps us realize the need to keep our liver healthy. We should also deal with any root causes quickly.
Key Takeaways
- Liver fibrosis and cirrhosis represent different stages of liver damage, with fibrosis potentially reversible.
- Factors influencing liver disease progression include age, alcohol consumption, and body mass index.
- Effective biomarkers play a crucial role in assessing liver health and gauging treatment responses.
- The METAVIR scoring system categorizes fibrosis into five distinct stages.
- Timely detection and management of liver fibrosis can prevent further complications, including cirrhosis.
What is Liver Fibrosis?
Liver fibrosis is when too much collagen and other proteins build up in the liver. This often comes from chronic liver inflammation. It’s important because it shows how ongoing inflammation can damage the liver’s structure.
Definition and Overview
Liver fibrosis means normal liver tissue is replaced by scar tissue due to injury. This can happen without any symptoms until it’s quite advanced. Catching and treating fibrosis early can sometimes reverse the damage.
Causes of Fibrosis Development
Many things can cause fibrosis, like:
- Chronic viral hepatitis (Hepatitis B and C)
- Alcohol-related liver disease
- Non-alcoholic fatty liver disease (NAFLD)
- Autoimmune liver diseases
- Biliary diseases, such as Primary Biliary Cholangitis
- Genetic disorders, particularly haemochromatosis
These conditions lead to ongoing inflammation, which can create a setting where fibrosis develops. Knowing these causes is key to stopping fibrosis before it gets worse.
The Dynamics of Hepatic Fibrogenesis
The process of hepatic fibrogenesis is a complex mix of cellular actions. These actions lead to liver fibrosis. At the heart of this is how collagen plays a role in fibrosis.
Collagen buildup turns into scar tissue. This is mainly due to activated hepatic stellate cells (HSCs) and myofibroblasts. When the liver gets injured, these cells spring into action. They are key in the formation of fibrosis.
Role of Collagen in Scar Tissue Formation
Collagen is vital for the structure of the liver. During fibrosis, we see collagen’s role in fibrosis through too much deposition. This messes up the liver’s normal structure.
Myofibroblasts pump out a lot of collagen I, damaging the extracellular matrix (ECM). The switch-on of HSCs, often by TGF-β1, is crucial for the increase in collagen. As a result, fibrous bands form. These bands cause liver stiffness, leading to chronic damage and problems.
Key Cellular Players in Fibrosis
The cellular players in liver fibrosis greatly influence hepatic fibrogenesis. These include:
- Hepatic Stellate Cells (HSCs): Initially inactive, these cells activate after liver damage. They then change into cells that produce ECM.
- Macrophages: These cells are big sources of pro-fibrotic cytokines like TGF-β1. They help keep fibrosis going through inflammation.
- Bone Marrow-derived Stem Cells: During liver damage, these cells may join the myofibroblast group. They play different roles in fibrosis.
To sum up, knowing how hepatic fibrogenesis works is vital. This includes understanding both collagen and cellular roles. This knowledge can guide us towards new treatments. Research is ongoing and continues to shed light on how the liver responds to injury. This brings both new challenges and avenues in treating liver fibrosis.
The Stages of Liver Fibrosis
The journey through liver fibrosis begins at stage F0, showing no signs of fibrosis, and can advance to stage F4, which means cirrhosis. These stages help us understand how severe liver damage is and its effects on health. Knowing these stages aids in liver fibrosis assessment using different fibrosis scoring systems.
Scoring Systems and Assessment
The METAVIR system is one way doctors can classify liver fibrosis. It scores inflammation from A0 to A3 and fibrosis from F0 to F4. This helps in understanding the liver’s condition.
The International Association of the Study of the Liver (IASL) has another system. It looks at fibrosis severity in chronic hepatitis. Knowing these systems helps doctors assess liver disease risks. It’s important for people, especially those with higher risk factors, to have regular check-ups.
Overview of Common Scoring Systems
There are a few main scoring systems used by doctors:
| Scoring System | Grades for Inflammation | Stages of Fibrosis |
|---|---|---|
| METAVIR | A0 to A3 | F0 to F4 |
| Knodell | 0 to 18 | 0 to 4 |
| Ishak | 0 to 6 | 0 to 6 |
These systems are key for setting the right treatment plans. Using them right helps patients get better results. For more info on liver issues and pain, check out this link: exploring liver pain causes.
Progression from Fibrosis to Cirrhosis
The change from liver fibrosis to cirrhosis is a major health shift. It is driven by several key factors. Knowing these factors helps prevent more damage and start early help. It’s vital to watch liver health closely because many things can speed up fibrosis.
Factors Leading to Progression
Many things can make liver fibrosis turn into cirrhosis faster. These include:
- Excessive alcohol consumption
- Obesity, leading to non-alcoholic fatty liver disease (NAFLD)
- Viral infections, especially hepatitis B and C
- Long-term inflammation and autoimmune diseases that affect the liver
NAFLD impacts about 25% of adults globally. This shows how it plays a part in liver fibrosis. The threat of moving to cirrhosis is serious. About 20% with NASH and severe fibrosis might get cirrhosis in two years.
Long-term Consequences of Liver Scarring
Liver fibrosis getting worse means more serious consequences. Long-term effects of cirrhosis include:
- Liver not working well or failure
- Portal hypertension, leading to problems like varices and ascites
- Higher chance of getting a common liver cancer called hepatocellular carcinoma
About 21% with NAFLD face fast move to severe fibrosis in six years. Serum markers are key for tracking this. For instance, HVPG tests show the risk of liver issues getting worse. Higher results point to bigger risks.
It’s key to manage these risks early by getting regular checks and being proactive in healthcare. People with NASH or severe fibrosis should look into treatments. This might include joining clinical studies to keep their liver healthy. For more info, check out this resource.
Symptoms of Advanced Liver Fibrosis
Advanced liver fibrosis can show symptoms that might be hard to spot at first. This makes it very important to catch the signs early. If not, many people don’t realize they have it until it’s quite advanced. Knowing the symptoms can lead to faster help and better outcomes.
Common Signs and Indicators
As the liver gets more damaged, symptoms of advanced fibrosis will show up. You might notice things like:
- Fatigue – A deep tiredness that rest doesn’t help.
- Swelling – Fluid buildup causing swelling in legs, ankles, or belly.
- Abdominal discomfort – Pain or discomfort in the upper right abdomen area.
- Nausea and vomiting – Unexplained nausea or vomiting.
- Weight loss – Losing weight without trying because of less appetite.
- Easy bleeding or bruising – Bleeding or bruising easily could mean liver trouble.
- Jaundice – Yellowing skin and eyes from bile buildup.
Importance of Early Detection
Many people don’t show early symptoms of liver fibrosis. This makes regular checks vital, especially for those at risk. Finding it early boosts chances for managing the disease well. Stopping the cause, like hepatitis or too much alcohol, can help prevent worse conditions like cirrhosis.
Knowing what puts you at risk and the symptoms can make a big difference. Getting checked early if you notice any symptoms can help keep your liver healthy longer.
| Symptom | Description |
|---|---|
| Fatigue | Persistent tiredness despite adequate rest. |
| Swelling | Fluid retention, especially in the legs and abdomen. |
| Abdominal discomfort | Pain in the upper-right side of the abdomen. |
| Nausea and vomiting | Repeated sensations of nausea and instances of vomiting. |
| Weight loss | Loss of weight due to poor appetite or nutrient absorption. |
| Easy bleeding | Unusual bruising or bleeding due to clotting issues. |
| Jaundice | Yellow discoloration of the skin and eyes. |
Assessing Liver Health
Checking liver health is very important for early diagnosis and treatment of liver problems. Various liver biopsy methods have been used for this. But, they have downsides like being invasive and sometimes not accurate. Lately, fewer liver biopsies are being done for routine checks of hepatitis B and C. There is more interest in less harsh ways of diagnosing.
Liver Biopsy vs. Non-invasive Tests
Liver biopsies give useful info but can be painful. They also have risks like bleeding or infection. On the other hand, non-invasive fibrosis tests are becoming popular. Tests like FibroScan and blood biomarkers are used. They have proven to be good at finding serious fibrosis and cirrhosis. For example, the Forns Index has an 88% success rate in spotting significant fibrosis. The APRI test has an 81% success rate, showing these methods are effective.
Emerging Diagnostic Modalities
New tools for checking liver health are being developed. These include future markers to make non-invasive tests better. One big advantage is they allow doctors to watch fibrosis progression over time. This means patients don’t have to go through invasive tests. As we learn more about liver disorders, focusing on good liver health assessments is crucial. This helps avoid severe issues like cirrhosis, which impacts healthcare costs and patient survival. For more details on these diagnostic improvements, check out this resource: liver biopsy methods and non-invasive alternatives.

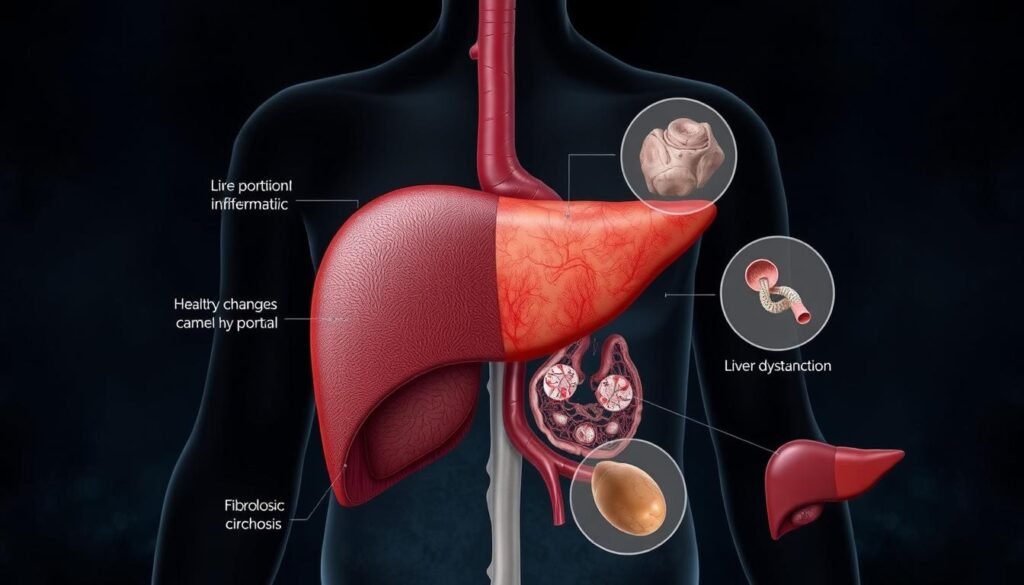
Understanding Cirrhosis Development
Cirrhosis is a major health issue caused by chronic liver diseases that lead to severe scarring. It brings about many changes in the liver, showing its deep impact on health. Knowing what cirrhosis is and how it happens is key for early help and care.
Definition and Pathophysiology
Cirrhosis is defined by scar tissue and changed blood flow in the liver. The liver changes, leading to problems like portal hypertension, ascites, and brain issues. There are two types of cirrhosis: one where symptoms are manageable and another where they’re severe.
Some with light symptoms can live many years without needing a new liver. This fact comes from research on liver failure stages. For more info, check this guide.
Risk Factors for Developing Cirrhosis
It’s important to know what causes cirrhosis to prevent and watch for it. Causes include chronic viral infections, too much alcohol, and genetics. Going for regular medical checks can help lower these risks and keep the liver healthy.
The severity of cirrhosis is measured with tools like the Child-Pugh score and MELD. These tools guide treatment choices and how urgent a liver transplant might be. Learn more about liver fibrosis and its progression here.
Impact of Cirrhosis on Health
Cirrhosis can strongly affect your health because it comes with complications. These problems include portal hypertension and a higher chance of getting liver cancer. Knowing about these issues helps in dealing with cirrhosis better.
Portal Hypertension and Its Complications
Portal hypertension is a major issue caused by cirrhosis. It happens when scar tissue blocks blood flow through the liver. This blockage leads to serious problems, such as:
- Variceal bleeding: This is when veins in the esophagus or stomach get too big and burst, which is very risky.
- Ascites: This is when fluid builds up in the belly, making it uncomfortable and more prone to infections.
- Spontaneous bacterial peritonitis: This is a dangerous infection in people with ascites, and it needs quick treatment.
It’s important to keep an eye on these issues if you have cirrhosis. This helps lessen the health problems it causes.
Risk of Hepatocellular Carcinoma
Having cirrhosis also means you have a higher risk of getting liver cancer, especially hepatocellular carcinoma. Regular check-ups are crucial because liver cancer often starts in people who already have cirrhosis. Doctors usually suggest:
- Ultrasound imaging: Getting liver ultrasounds regularly helps catch cancer early on.
- Alpha-fetoprotein blood tests: Checking this tumor marker helps spot cancer risks sooner.
Dealing with these issues early makes managing liver cancer risk better for those with cirrhosis. Prevention and early spotting are key for healthy living with this condition.
Treatment and Management Strategies
Liver fibrosis treatment tackles ways to reverse fibrosis and deal with its causes. The approach depends on what’s causing the liver damage. Even though it’s slow, the goal is to stop fibrosis from getting worse and make the liver healthier.
Interventions for Reversing Fibrosis
Doctors are looking into various treatments to potentially reverse liver fibrosis. These include:
- Antiviral Therapies: These focus on viral hepatitis to help the liver heal and stop more damage.
- Dietary Supplementation: Some nutrients and antioxidants might improve liver function and lessen inflammation.
- Biological Treatments: New therapies are trying to change the immune response and fibrosis process.
- Stem Cell Transplantation: This method works to fix damaged liver cells and bring back normal function.
- Genetic Regulation: Altering gene expressions could be another way to treat effectively.
Importance of Addressing Underlying Causes
To really tackle liver fibrosis, it’s crucial to deal with what’s causing it. Here are the main steps:
- Avoid alcohol, which is vital for people with cirrhosis.
- Be careful with drugs. For instance, acetaminophen is safer in small amounts.
- Make diet changes. Try to keep salt under two grams a day to manage health better.
- Get vaccinated against hepatitis A and B, plus the regular flu shots.
- Talk to doctors about your symptoms, past treatments, and any supplements to plan the best strategy.
The journey to beat liver fibrosis includes many steps and might not clear fibrosis entirely in severe cases. However, a good management plan and changing lifestyles can greatly improve how well treatments work and decrease liver disease risks.
Delving Into Related Complications
Cirrhosis is a major health issue, leading to various complications. Among them, esophageal varices and ascites stand out. They can greatly affect a person’s life. Managing these conditions is key for those dealing with cirrhosis.
Esophageal Varices and Ascites
Esophageal varices come about due to high pressure in the portal vein from liver damage. They could cause dangerous bleeding. On the other hand, ascites involves fluid build-up in the belly. It causes discomfort and more issues due to similar pressure increases.
Management of Complications Associated with Cirrhosis
Managing esophageal varices includes:
- Endoscopic band ligation to stop bleeding.
- Beta-blockers to lower pressure in veins.
Treating ascites mainly involves:
- Diuretics to cut down on fluid buildup.
- Paracentesis to remove extra fluid, easing patients’ discomfort.
These methods show the need for full care. They address complications from cirrhosis and how they affect health.
Conclusion
The journey from fibrosis to cirrhosis shows why catching liver issues early matters. If we find fibrosis soon enough, treatments can really help. For example, getting phlebotomies for too much iron, or controlling chronic hepatitis, can turn fibrosis around. This way, we can stop cirrhosis before it starts, or even improve the liver’s status.
It’s vital to keep an eye on how fibrosis could turn into cirrhosis. People and doctors need to know what signs to watch for. By checking the liver regularly with safe tests, we can act fast if trouble shows up. Paying attention to what hurts the liver is key to keeping it healthy.
Even if we can’t fix all cirrhosis damage, we can make living with it better. Learning about liver health matters a lot. It helps people choose how to protect their liver and health. Starting early with these steps makes a big difference for your future.