About 25% of adults in the US have Fatty Liver Disease. This condition, also known as hepatic steatosis, is where too much fat builds up in the liver. If not addressed, it can turn into serious problems like inflammation and cirrhosis.
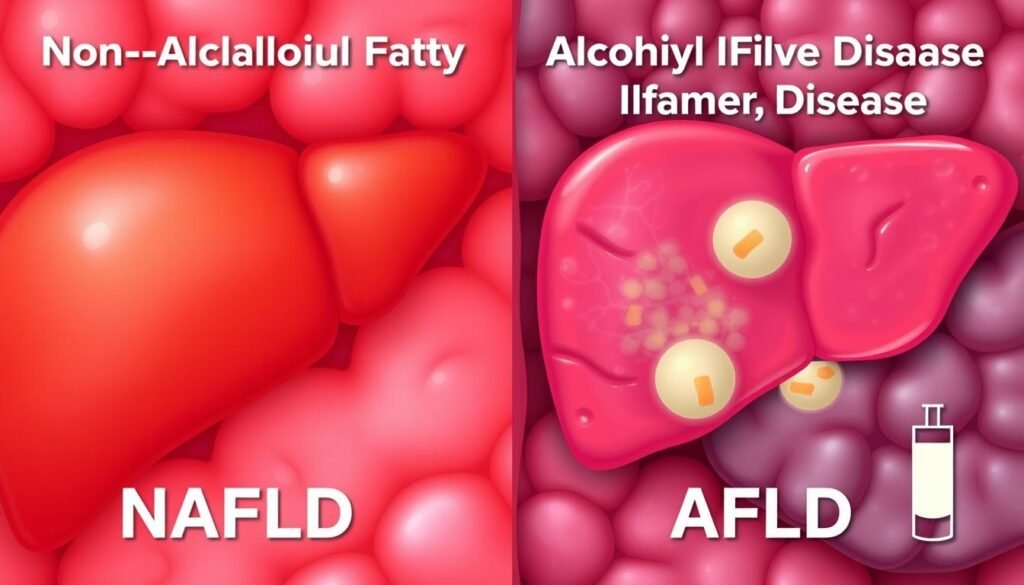
Fatty Liver Disease comes in two main types: Alcoholic (AFLD) and Nonalcoholic (NAFLD). The increase in these diseases is tied to bad lifestyle choices. It’s vital to catch the early signs to stop them from getting worse.
We will explore the causes, types, and important facts of Fatty Liver Disease. The goal is to understand how to fight this health issue effectively.
Key Takeaways
- Approximately 25% of U.S. adults are affected by Fatty Liver Disease.
- Hepatic steatosis can lead to serious complications, including liver inflammation.
- The two main types of Fatty Liver Disease are alcoholic and nonalcoholic.
- Recognizing early symptoms is critical for effective management.
- Unhealthy lifestyle choices significantly contribute to the rising prevalence.
What is Fatty Liver Disease?
Fatty Liver Disease happens when too much fat builds up in the liver. This condition, called hepatic steatosis, doesn’t always come from drinking alcohol. Fat in the liver can hurt its ability to work and might lead to swelling and more liver problems.
There are two main kinds of Fatty Liver Disease: Alcoholic Fatty Liver Disease (AFLD) and Nonalcoholic Fatty Liver Disease (NAFLD). Drinking too much alcohol causes AFLD. Factors like being overweight, diabetes, and metabolic syndrome are key in NAFLD.
If not dealt with early, Fatty Liver Disease can get worse. It can turn into cirrhosis or lead to liver cancer. Knowing about your liver health and spotting signs early can help stop these big problems.
To keep your liver healthy, eat right and be active. This is very important to stop and manage Fatty Liver Disease. Knowing about the disease helps people get medical advice early. This helps better their health overall.
Types of Fatty Liver Disease
Fatty liver disease is when too much fat builds up in the liver. There are two main kinds: Alcoholic Fatty Liver Disease and Nonalcoholic Fatty Liver Disease. It’s important to know the difference to treat them right.
Alcoholic Fatty Liver Disease (AFLD)
Drinking too much alcohol can cause Alcoholic Fatty Liver Disease. It’s an early sign of liver damage from alcohol. Continuing to drink can lead to worse problems like cirrhosis and liver cancer.
Symptoms include feeling tired, pain in the stomach, and yellowing skin. If someone is diagnosed, they must stop drinking alcohol to prevent more harm.
Nonalcoholic Fatty Liver Disease (NAFLD)
Nonalcoholic Fatty Liver Disease happens mostly in people who are overweight, have insulin resistance, or have metabolic syndrome. These people often drink little to no alcohol. They might feel tired or have pain in the upper stomach area.
Without treatment, NAFLD could get worse, becoming steatohepatitis or fibrosis. To get better, changing one’s lifestyle is key. This includes losing weight and eating healthier.
| Type of FLD | Cause | Common Symptoms | Risk Factors |
|---|---|---|---|
| Alcoholic Fatty Liver Disease | Excessive alcohol consumption | Fatigue, abdominal pain, jaundice | Heavy drinking, genetic predisposition |
| Nonalcoholic Fatty Liver Disease | Obesity, insulin resistance | Fatigue, abdominal discomfort | Obesity, diabetes, high cholesterol |
For more info about these liver conditions, click here. Learning about these types helps with prevention and better treatment.
Understanding Hepatic Steatosis
Hepatic Steatosis happens when too much fat builds up in the liver. This can deeply affect how the liver works, leading to various liver health problems. If the liver stores too much fat, it can mess up normal cell functions.
The liver is key in processing what we eat and drink. In a healthy liver, fat storage and use are well managed. But, too much fat can cause hepatic steatosis. This condition is different from other serious liver diseases like alcoholic liver disease and cirrhosis.
Knowing why fat gathers in the liver is critical. Factors like a poor diet or metabolic issues can lead to excess fat. If we eat more fat than the liver can handle, it starts to store too much.
Here’s a brief look at how hepatic steatosis progresses and its effect on the liver:
| Stage | Description | Impact on Liver Function |
|---|---|---|
| Early Stage | Initial fat buildup, often without symptoms. | Little to no effect on liver function. |
| Moderate Stage | More fat leads to possible inflammation. | Moderate disruption of liver function. |
| Advanced Stage | Excessive fat can damage the liver. | Greatly reduced liver function, risk of scarring. |
Dealing with hepatic steatosis early, through lifestyle or medical help, is key to keeping a healthy liver. Being aware of how diet and lifestyle impact fat in the liver can help us prevent liver issues.
Common Causes of Fatty Liver Disease
Fatty liver disease comes from different lifestyle and health factors. Knowing the causes can help us manage and prevent it. Main factors include obesity, insulin resistance, and a poor diet.
Obesity
Obesity is a key factor behind fatty liver disease. It happens when too much body fat increases liver fat levels. This can cause inflammation and scarring in the liver.
Studies link higher body mass index (BMI) to worse liver fat levels. It’s vital to address obesity to prevent liver damage.
Insulin Resistance
Insulin resistance is another major cause. It occurs when the body can’t handle sugars and fats well, leading to fat build-up in the liver. This often goes hand in hand with obesity, worsening both conditions.
People with insulin resistance have a greater risk of liver problems. Research backs this up.
Unhealthy Diet
A bad diet also leads to fatty liver disease. Eating lots of sugars, saturated fats, and processed foods is harmful. The standard American diet is too rich in these and lacks nutrients.
Studies show that bad food choices contribute to liver disease. Improving your diet is key to prevention and treatment.

Risk Factors for Developing Fatty Liver Disease
Knowing what leads to fatty liver disease is key to stopping it early. Many things can make a person more likely to get this illness. It’s important to know which factors impact vulnerability the most.
Genetics
Genes are big players in fatty liver disease. If your family has a history of liver issues, your risk goes up. Some genetic traits make people more prone to issues with their metabolism. This can affect liver health a lot.
Metabolic Syndrome
Metabolic syndrome includes problems like high blood pressure, sugar, waistline fat, and weird cholesterol levels. Each issue raises your risk for fatty liver. They all make it harder for your liver to handle fats and toxins. Knowing this, it’s smart to watch your health closely to reduce your risk.
Age and Gender
Different ages and genders have different risks for fatty liver. Usually, those over 50 have to be more careful. But, younger adults aren’t totally safe, especially if they have other risks. Men are generally more at risk, but post-menopausal women see their risk go up because of hormonal changes.
Symptoms of Fatty Liver Disease
Finding out if you have Fatty Liver Disease early is tough. Many people don’t see clear signs at first. You might feel really tired or have discomfort in your upper right belly. When the disease gets worse, the symptoms are more obvious because of liver harm.
As Fatty Liver Disease gets bad, you might notice:
- Unexplained weight loss
- Jaundice, seen as yellowing of the skin and eyes
- Swelling in the abdomen or legs
- Severe fatigue and weakness
It’s vital for people, especially those at risk, to keep an eye out. Going for regular doctor visits helps catch the disease early. This means you can manage symptoms better. For extra info on Fatty Liver Disease symptoms, medical guides are very helpful.
How is Fatty Liver Disease Diagnosed?
Fatty Liver Disease diagnosis starts with a deep look at medical history and a physical check-up. Doctors talk about symptoms, lifestyle, and risk factors. This helps decide if more tests are needed.
Medical History and Physical Examination
In the medical history talk, doctors ask about eating habits, drinking alcohol, and other health issues. A physical exam may show a bigger liver, leading to more checks. The aim is to find any signs of Fatty Liver Disease.
Imaging Tests and Blood Work
Imaging tests are key in spotting Fatty Liver Disease. Ultrasounds and MRIs picture the liver’s fat and structure. They show how much damage there is and point out the disease type.
Blood work is also crucial. It checks liver enzymes to see how the liver works and if it’s inflamed. High enzymes might mean early Fatty Liver Disease or its advance. Imaging and blood tests together give a full view of liver health.
| Test Type | Description | Purpose |
|---|---|---|
| Ultrasound | A non-invasive imaging technique using sound waves | To detect fat accumulation in the liver |
| MRI | An advanced imaging test providing detailed liver images | To evaluate the extent of liver damage |
| Blood Work | Tests measuring liver enzyme levels and overall function | To assess liver health and identify possible inflammation |
Complications Associated with Fatty Liver Disease
Fatty liver disease can lead to several serious complications if not treated. It can cause different, dangerous health issues. Knowing about these problems is key to seeking timely help and managing the condition well.
Liver Inflammation
Liver inflammation, or steatohepatitis, can start because of too much fat in the liver. This causes damage, leading to symptoms like tiredness, upper abdomen discomfort, and even jaundice. If this inflammation goes on for a long time, it can get much worse and lead to cirrhosis.
Cirrhosis
Cirrhosis is a severe stage of fatty liver disease. Here, ongoing liver damage causes a lot of scarring, which harms liver function. People with cirrhosis might face very serious issues like liver failure. Watching liver health closely can help catch cirrhosis early. This can open the door to protective steps.
Hepatocellular Carcinoma
Having cirrhosis increases the risk of getting a liver cancer called hepatocellular carcinoma. Research shows that cirrhosis from fatty liver disease makes liver cancer more likely. It’s crucial to take care of our liver health. For more details on fatty liver disease, diagnosis, and treatment, check out this detailed guide.
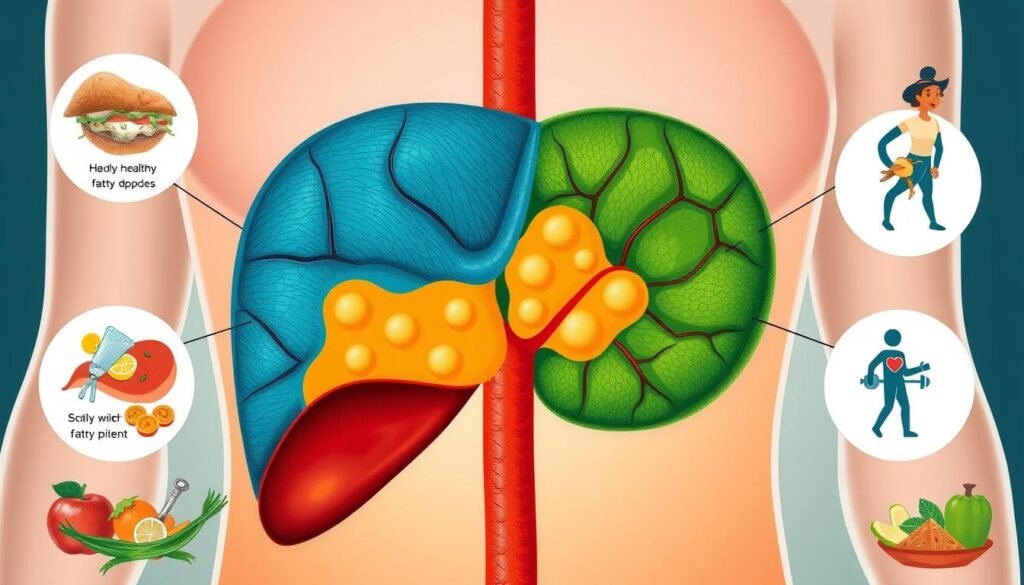
Management and Treatment Options for Fatty Liver Disease
Dealing with Fatty Liver Disease (FLD) means changing how you live and sometimes taking medicine. These steps can help improve your liver’s health and lower the risk of more problems.
Lifestyle Modifications
Making changes in your daily life is key to managing FLD. It’s important to eat a healthy diet full of fruits, veggies, lean meats, and whole grains. Avoiding high-fat, sugary, and processed foods is also crucial. Adding exercise like walking, swimming, or biking can help you lose weight and improve your metabolism. These changes help your liver and also fight obesity and insulin resistance.
Medications
While changing your lifestyle is the core of managing FLD, some people might also need medicine. Researchers are looking at drugs that could help, such as pioglitazone and vitamin E for those without diabetes. Always talk to a doctor to find the right treatment plan for you.