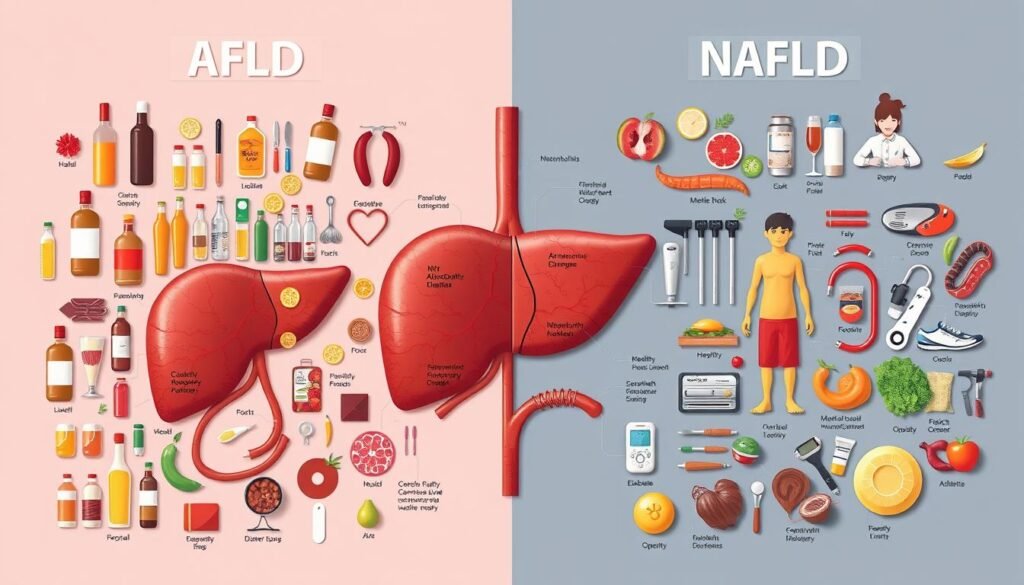
Have you ever thought about how lifestyle choices can lead to severe liver diseases? Often, these diseases show no noticeable symptoms. The difference between Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD) highlights the impact of diet, alcohol, and health on our livers. This article will compare the causes, symptoms, and treatments of these two conditions that impact millions worldwide.
Key Takeaways
- AFLD typically arises from excessive alcohol consumption, while NAFLD is related to obesity and diabetes.
- NAFLD affects nearly 10% of children in the United States, highlighting its growing prevalence.
- Many individuals with AFLD display symptoms only after significant liver damage has occurred.
- Weight loss and lifestyle modifications can significantly improve NAFLD, reducing steatosis and even resolving non-alcoholic steatohepatitis (NASH).
- Collaboration between researchers and industries is essential to develop effective therapies for both AFLD and NAFLD.
Introduction to Fatty Liver Diseases
Fatty liver diseases are conditions with too much fat in the liver. There are two main types: Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD). They are key parts of metabolic syndrome, a major public health issue. These diseases also add a lot to healthcare costs due to their increasing numbers.
NAFLD shows how metabolic syndrome affects the liver. It’s linked with obesity and type 2 diabetes. A recent study shows about 25% of adults worldwide have NAFLD. This number varies between 12.9% to 46% in places like Europe, the United States, and Asia. This shows the need to understand what causes liver inflammation.
Lately, there’s been a rise in liver cirrhosis due to AFLD and NAFLD. Around 48% of cirrhosis deaths worldwide are from AFLD. This points to the serious outcomes of chronic liver diseases. Experts think liver problems will much more common by 2030, possibly doubling or tripling.
The ages people get liver diseases differ. In the U.S., most AFLD hospital visits are from people aged 45 to 69. In Japan, NAFLD affects different ages and genders differently. More men have these liver issues, with men to women ratios being 9:1 for alcoholic liver cirrhosis.
Ethnic differences also affect who gets fatty liver diseases. Hispanic people have higher rates than non-Hispanic Whites and Blacks. Genes, lifestyle, and where you live all play a part. It’s important to get why this happens to stop and treat these diseases better.
What is Alcoholic Fatty Liver Disease (AFLD)?
AFLD happens when too much drinking leads to fat build-up in liver cells. This fat build-up is the first sign of liver damage from drinking. Knowing what causes AFLD is important. It helps people understand how to avoid excessive alcohol and keep their liver healthy.
Causes of AFLD
Drinking too much alcohol is the main cause of AFLD. If someone drinks heavily over time, their risk of liver harm goes up. This leads to fat being stored in liver cells. Factors that add to this risk include:
- Prolonged heavy drinking patterns
- Genetic factors that make some more vulnerable
- Gender, with men more often at risk
- Other health issues that could make liver damage worse
Studies show that more than 90% of heavy drinkers might get liver damage. This shows how alcohol is a key factor in AFLD. Knowing these causes helps stop more liver problems.
Symptoms of AFLD
At first, AFLD might not show any signs, making it hard to spot early. Signs can be different for everyone. Yet, some common ones include:
- Fatigue
- Abdominal discomfort
- Jaundice, in advanced cases
Liver tests may show high liver enzymes, a sign of liver cell harm. Without treatment, AFLD can get worse, leading to cirrhosis or liver cancer. Being aware of these symptoms is key to early AFLD care.
What is Non-Alcoholic Fatty Liver Disease (NAFLD)?
NAFLD stands for non-alcoholic fatty liver disease. It is when fat builds up in the liver of people who drink little or no alcohol. It’s now the most common liver disease worldwide, affecting about one-third of adults. This issue is especially common in Western countries, with rising obesity numbers playing a big part.
Causes of NAFLD
Mostly, NAFLD is caused by things that make up metabolic syndrome. This includes obesity, insulin resistance, and type 2 diabetes. In fact, 75-92% of obese folks might have NAFLD. There are other factors too:
- Genetic predisposition
- Gut microbiota imbalance
- High cholesterol or triglycerides
- Medical conditions such as hypothyroidism
- Age over 50
Even people who don’t fit the usual risk profile can get NAFLD. This shows how complex the disease is.
Symptoms of NAFLD
Many with NAFLD don’t feel sick. Some might feel tired, unwell, or have discomfort in the upper right stomach area. Often, doctors find out someone has NAFLD when liver tests show high enzymes. If not dealt with, it can get worse, leading to serious liver diseases like NASH, cirrhosis, or liver cancer.
| Condition | Prevalence | Common Risk Factors |
|---|---|---|
| NAFLD | 25% – 33% of adults | Obesity, Insulin Resistance, Genetics |
| NASH | 1.5% – 6.5% of adults | Age, Obesity, Diabetes |
| MAFLD | 15.3% – 34% | Similar to NAFLD, but with advanced fibrosis risk |
AFLD vs. NAFLD Comparison
The AFLD vs. NAFLD comparison highlights important talks on both conditions. They both impact the liver but differ significantly. The pathophysiological differences and risk factors set them apart.
Pathophysiological Differences
AFLD mainly involves liver steatosis, inflammation, and oxidative stress from alcohol. This causes inflammation that’s more severe than NAFLD. NAFLD, on the other hand, is mostly about fat build-up due to metabolic issues. Each has its own disease progress.
These differences mean we must tailor treatment and care strategies for each condition. It’s important to understand how they affect the liver differently.
Risk Factors for AFLD and NAFLD
Risk factors play a big role in how common and severe AFLD and NAFLD are. In Finland, 21% had NAFLD, but only 7% had AFLD. Drinking is a major risk for AFLD, especially in males aged 45 to 70. NAFLD is linked with obesity, metabolic issues, and not moving enough.
Interestingly, metabolic syndrome is slightly more common in AFLD (73%) than in NAFLD (70%). Both conditions often occur with type 2 diabetes, affecting around 24-25% of people. Knowing these risk factors helps us prevent and improve care for these patients.
For more info on AFLD and NAFLD, including debates on their definitions and management, check out this article.
Diagnosis of AFLD and NAFLD
Diagnosing Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD) can be tough. They have similar symptoms. Doctors pay close attention to a patient’s history. They look at alcohol use for AFLD and metabolic problems for NAFLD.
Doctors use imaging like ultrasound, MRI, and CT scans to see the liver. These methods are helpful but they can’t confirm everything. A liver biopsy, though, can tell doctors a lot. They can look at liver tissue to figure out the exact problem.
If someone is at risk, a liver biopsy might be needed. Knowing the exact type of liver disease helps decide on treatment. Tests can also show how much the liver is damaged and if more help is needed.
Getting a clear diagnosis involves looking at a patient’s history, using imaging, and sometimes a liver biopsy. This way, doctors can better handle AFLD and NAFLD.
Clinical Features of AFLD
Understanding the signs of Alcoholic Fatty Liver Disease (AFLD) is key for diagnosis and care. This condition shows various symptoms that indicate the health of the liver. These symptoms help tell it apart from other liver diseases. Detecting it early is vital for better results for patients.
Key Indicators and Biomarkers
Important signs of AFLD are high levels of certain liver enzymes. These include aspartate aminotransferase (AST) and alanine aminotransferase (ALT). High levels of these enzymes show liver inflammation and damage. An AST/ALT ratio above 2:1 points to damage from alcohol.
More signs are longer prothrombin time and high blood pressure. This might mean liver problems and changes linked to AFLD. Checking these signs and biomarkers helps understand the disease’s seriousness. This guides in choosing the right treatments.
It’s crucial to monitor these indicators. People with AFLD might face a higher chance of getting type 2 diabetes and metabolic syndrome. This is due to liver issues. Regular checks and changes in lifestyle are advised to better liver health and reduce risks.
| Clinical Feature | Description |
|---|---|
| Liver Enzymes (AST, ALT) | Elevated levels indicate liver inflammation or injury. |
| AST/ALT Ratio | Greater than 2:1 suggests alcoholic liver damage. |
| Prothrombin Time | Prolonged time may reflect impaired liver function. |
| Hypertension | Commonly observed in patients with fatty liver. |
Knowing these signs is crucial for treating AFLD patients effectively. It ensures they get care that focuses on keeping the liver healthy and improving well-being. To learn more about liver health, see this resource.
Clinical Features of NAFLD
Non-Alcoholic Fatty Liver Disease (NAFLD) impacts health and life quality in big ways. It often includes signs like obesity, high blood pressure, and insulin resistance. Knowing these signs helps manage the disease better.
Key Indicators and Biomarkers
Important signs of NAFLD are found through liver function tests and scans. Biomarkers are crucial for diagnosing and tracking it. High levels of ALT and AST suggest liver inflammation or damage. Scans usually reveal hepatic steatosis, meaning too much fat in the liver.
NAFLD’s prevalence varies, from 12.9% to 46.0% across different places like Europe, the USA, and Asia. Rates are higher in Hispanics than other groups. Obesity is common in 75-92% of those with NAFLD. This shows the need to focus on specific risks for certain populations.
Finding NAFLD early is key. Anyone with symptoms or risk factors should get regular liver function tests and check for metabolic syndrome. Knowing about biomarkers and their link to liver health helps in making better prevention and treatment plans.
For more details, check on how to manage liver health and avoid complications from long-term liver inflammation. Seek medical attention when needed, and make lifestyle changes.
Progression and Outcomes
The relationship between AFLD and NAFLD shows clear differences. Alcoholic Fatty Liver Disease often results in serious conditions like cirrhosis and cancer more than NAFLD does. Studies show 20% of AFLD patients get cirrhosis, but only 7% of those with NAFLD do. This shows how harmful alcohol can be to the liver.
The reason for these disease differences comes from how they damage the liver. Alcohol directly harms the liver in AFLD patients, causing quicker damage. NAFLD is related to metabolic issues and obesity, leading to slower damage that appears in late stages.
Survival rates also differ between the diseases. NAFLD patients have a median survival of 24 years, while AFLD patients have 20 years. Also, 36% of AFLD patients die from liver disease, compared to 7% of NAFLD patients. This shows the harsh impact of each disease.
The risk factors for disease progression show more differences. Both diseases see worse survival with severe fibrosis, with a hazard ratio of 2.09. Understanding these factors is vital for better treatments and outcomes.
| Parameter | AFLD | NAFLD |
|---|---|---|
| Median Survival (years) | 20 | 24 |
| Rate of Liver Cirrhosis (%) | 20 | 7 |
| Leading Cause of Death (%) | Liver Disease (36) | Cardiovascular Disease (48) |
| Liver-Related Death Rate (%) | 36 | 7 |
| Fibrosis Impact on Survival | HR 2.09 | HR 2.09 |
Available Treatments for AFLD
Managing Alcoholic Fatty Liver Disease (AFLD) involves multiple steps. The main goal in treating AFLD is to stop drinking alcohol. This is key to getting better. Along with quitting alcohol, eating right helps support the liver. Both are vital in fighting inflammation and healing.
Current Management Strategies
Today’s strategies to fight AFLD include:
- Abstinence: Not drinking alcohol at all is essential for healing.
- Nutritional Therapy: Eating a balanced diet helps the liver repair itself.
- Corticosteroids: In some cases, these drugs are used to lessen liver swelling.
- Lifestyle Modifications: Adding exercise and managing weight also helps improve health.
However, not all patients get better with these treatments. For those who don’t, research is finding new ways to help.
Future Therapies in Development
There’s exciting research for new AFLD treatments. Studies are looking into things like probiotics, antioxidants, and drugs that manage fats in the body. Scientists are working to better treatment results by understanding liver disease better. Knowing more about inflammation in AFLD could lead to new ways to protect and heal the liver. For more details on research, check out this article.
Available Treatments for NAFLD
Non-Alcoholic Fatty Liver Disease (NAFLD) is common, often seen with metabolic disorders like diabetes. The main treatments focus on lifestyle and diet changes to cut liver fat and boost health. It’s key to see how these can help with weight loss and liver well-being.
Lifestyle Modifications and Dietary Changes
Changing your lifestyle is key in handling NAFLD. Adding regular workouts and altering what you eat can really help. Studies reveal that losing 5% to 10% of your weight can decrease liver fat and lessen inflammation.
- The Mediterranean diet, known for its good fats, fruits, and veggies, helps reduce liver fat and improve insulin sensitivity.
- Working out can lower liver fat by 20–30% even without losing weight.
- People who are overweight or obese should aim for a 5% to 10% weight loss.
- Even non-obese individuals could see NAFLD go away with a 3% to 10% weight loss.
Medications and Interventions
While there’s no drug made just for NAFLD, new studies look at treatments for related issues like diabetes. Potential treatments include:
- Thiazolidinediones, which might help liver function and weight control.
- GLP-1 receptor agonists, good for handling diabetes, could also aid liver health and metabolic health through weight loss.
Given NAFLD’s rise, especially with type 2 diabetes, combining lifestyle changes with medical treatments could offer a full strategy against this illness.

Long-term Prognosis of AFLD and NAFLD
For those diagnosed with AFLD or NAFLD, the future can vary a lot. It depends on how their disease changes and their treatment results. Studies have found that people with NAFLD live about 24 years on average. Those with AFLD often live around 20 years. In the beginning, both conditions have similar five-year survival rates. Yet, as the disease gets worse, their paths diverge.
About 7% of NAFLD patients will develop cirrhosis. But this number jumps to 20% for AFLD patients. This shows how serious liver disease from too much alcohol can be. In NAFLD patients, almost half of the deaths are due to heart disease. Yet, for AFLD patients, liver disease is the main killer, causing 36% of deaths. Also, 7% of deaths in NAFLD patients are from liver issues. This is way higher than the overall death rate from liver disease, which is only 0.1%.
Looking at survival, AFLD patients have it tougher than NAFLD patients. This is clear from a hazard ratio (HR) of 2.16. When the liver fibrosis is moderate to severe, survival rates drop even more. This shows how crucial the disease’s severity is for long-term outcomes.
| Key Statistics | NAFLD | AFLD |
|---|---|---|
| Median Survival | 24 years | 20 years |
| Cirrhosis Development | 7% | 20% |
| Common Cause of Death | Cardiovascular Disease (48%) | Liver Disease (36%) |
| Liver-Related Deaths | 7% | Data unavailable |
| Hazard Ratio for Survival (AFLD vs. NAFLD) | 1.0 | 2.16 |
Conclusion
It’s important to know the difference between Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD). About 25% of people worldwide are impacted by these conditions. This calls for a broad strategy, focusing on lifestyle and medical treatments. Comparing AFLD and NAFLD shows their clinical similarities and distinct causes. Knowing this helps manage each disease correctly.
Simple steatosis can evolve into advanced cirrhosis or even lead to cancer. Recognizing the unique characteristics of each liver disease is crucial. Genetics and where a patient comes from also affect the disease. Doctors must consider these factors when treating fatty liver. As we learn more about these diseases, it becomes more critical to find interventions that work.
Research plays a big part in understanding AFLD and NAFLD. By looking into genetics, lifestyle, and environmental factors, better prevention and treatment plans can be made. A deeper knowledge helps improve patient care. It also helps tackle the global issue of liver diseases.